
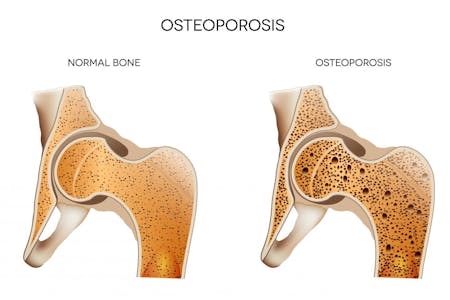
Osteoporosis literally translates to "porous bone". It is a bone condition where bones become weak and brittle due to the loss of bone mineral density and structure. Under a microscope, bones look like dense honeycombs. Bones weakened by osteoporosis have much larger holes and spaces within the honeycomb structure.
Osteopenia is basically the precursor to osteoporosis. A person with osteopenia has low bone density (low bone mass) but not to the point where it has developed into osteoporosis. According to the National Osteoporosis Foundation, approximately 33.6 million American adults (21.8 million American women and 11.8 million men) have osteopenia.
What is my Risk for Osteopenia and Osteoporosis?
Bones are living structures that change over a person's lifespan. They are at their peak density in people who are between 30 and 35 years of age. Then, they start losing bone mass. Osteopenia and osteoporosis typically occur in people over the age of 50. The age of onset depends on how healthy your bones were at their peak.
Some people with dense, healthy bones may not ever be affected by osteopenia or osteoporosis. People with a family history of osteopenia and osteoporosis are more prone to get it. Women, smaller-boned people, Caucasians and Asians are also more prone to osteopenia and osteoporosis than men, larger-boned females and people of other ethnicities.
Other causes include:
- Hormonal changes such as changes that occur in women after menopause and Andropause, the male equivalent of menopause, as well as high levels of cortisol, insulin and parathyroid hormone
- Smoking
- Consumption of caffeinated beverage (e.g., coffee), carbonated beverages (e.g., sodas, champagne, sparkling water, etc.) and excess consumption of alcohol
- Immobility due to frail health or lack of exercise
- Taking certain medications, including corticosteroids and anticonvulsant/anti-seizure medications
- Chronic inflammatory conditions, such as Rheumatoid Arthritis (RA)
- Malabsorption as a result of untreated Celiac Sprue
- Eating disorders, such as anorexia nervosa and bulimia
- Hyperthyroidism
- Vitamin D deficiency
- Taking acid-blocking drugs (e.g., Nexium, Protonix, Prevacid, Tagamet, and Zantac)
If you are a female over the age of 65 or you are at high risk for osteopenia and have suffered a fracture, you should request a bone mineral density (BMD) test from your healthcare provider. This is particularly important if you fractured a bone without trauma or by falling from a standing position. If you have osteopenia, your doctor will most likely schedule you for regular bone mineral tests every 2 to 5 years.
Early diagnosis and treatment of osteopenia are important and can help prevent osteoporosis and complications resulting from it. People with osteopenia are at higher risk for osteoporosis, a much more serious condition that can lead to fractures, hunched over posture and possibly severe pain.
Physical Therapy for Osteopenia and Osteoporosis
The goal of physical therapy for osteopenia and osteoporosis is to enhance bone mineral density and slow, or better yet, prevent the deterioration of bone mass (density). Treatment typically consists of physical therapist supervised weight-bearing exercises because these are the best way to strengthen your bones and muscles, while reducing your risk of fracture.
Lower extremity exercises alone can help increase the BMD of the hip and great trochanter but have little effect on the spine. However, when combined with upper body exercises, there is a much more significant increase of BMD in the spine in pre-menopausal females and pre-Andropause males. Weight-bearing exercise therapy may or may not increase BMD in post-menopausal women and post-Andropause men. However, it has proven to be valuable in reducing the rate of bone deterioration.
The reason exercise works is because it strengthens bones and muscles. Plus, it also improves balance, coordination and flexibility, which is key in preventing falls that can cause painful fractures. We will design a program that is best for you and your level of osteopenia or osteoporosis.
The exercise plan we design will focus on your body mechanics and posture, balance, resistance weights and other techniques to help improve your bone health or at least slow down the rate of deterioration. Your exercise therapy plan may consist of a combination of high-impact and low-impact weight-bearing exercises or just low-impact exercises, depending on several factors including:
- Fracture Risk
- Muscle Strength
- Current Level of Physical Activity and Fitness
- Gait, Balance and Flexibility / Range of Motion (ROM)
- Other Health Factors That May Affect Your Ability to Exercise (e.g., high blood pressure (HBP), heart conditions, obesity, mobility limitations, etc.)
Meet Your Therapists

Jennifer Rice, DPT - Physical Therapist
Jennifer graduated from Pennsylvania States University with a Bachelor's Degree in Kinesiology, then became a Certified Athletic Trainer. She continued her education at MCP Hahnemann University graduating with a Doctorate Degree in Physical Therapy. She is a member of the American Physical Therapy Association (APTA) and Pennsylvania Physical Therapy Association (PPTA). Jennifer's areas of expertise include post-surgical orthopedic and spine patients, women's health issues and recreation or competitive athletes. She is a Peer Educator for American Bone Health and has developed the most prominent Osteoporosis Program in Lancaster County with the Drevna-Hudson women's team. This well-known program focuses on prevention, education, exercise, and community engagement. Jennifer speaks on the topic of Osteoporosis at the community level.

Amy Humphrey, DPT, OCS, MTC - Physical Therapist
Amy graduated from Pennsylvania States University with a Bachelor of Science degree in Rehabilitation Services Education. She continued her education at Central Pennsylvania College where she received her Associate's Degree as a Physical Therapist Assistant in 1999. Amy's areas of expertise are aquatics, geriatrics, basic healthy living and nutritional based education, lymphedema, orthopedic care, tai chi, and women's health reiki. She is also a Peer Educator for American Bone Health and is an outstanding contributor to the prominent Osteoporosis Program at Drevna-Hudson Physical Therapy. This program focuses on prevention, education, exercise, and community engagement. She speaks on the topic of Osteoporosis at the community level.

Sherri Gagné, PTA - Physical Therapist Assistant
Sherri graduated from Eastern Mennonite University with a Bachelor of Science in Liberal Arts in 2000. She continued her education at Central Pennsylvania College with her Associate's degree as a Physical Therapist Assistant in 2006. Sherri's areas of expertise is with outpatient orthopedics however she is also a key contributor to the Drevna-Hudson Physical Therapy well-known Osteoporosis Program.

Bernadette Sheaffer, PTA - Physical Therapist Assistant
Bernadette is a 1990 graduate of IUP with a BS in Business Management. She went on to get her Physical Therapist Assistant degree from Central Penn College in 2019. Bernadette currently holds several certifications that contribute to her passion in overall health and wellness: NETA Personal Trainer, Schwinn Cycle Instructor, Les Mills Sprint Cycle Instructor, Mat Pilates Instructor and NASM Senior Fitness Specialist. She is also a Certified Peer Educator for American Bone Health and a prominent contributor to the Drevna-Hudson Physical Therapy well-known Osteoporosis Program.
Have you been diagnosed with osteopenia or osteoporosis? Call us to set up an appointment for an evaluation: (717) 569-4184. We'll set you up with a plan that's right for you!
